What is Dry AMD?
There are two kinds of AMD – dry and wet. The most common form of AMD is dry AMD, of which 85-90 percent of AMD patients are diagnosed. Dry AMD is caused by the appearance of small yellow deposits called drusen, which form under the retina. These are accumulated waste products of the retina, which can grow in size. This can cause the retinal cells in the macula that process light to die, causing vision to become blurred. This form of the disease usually worsens slowly.
There are three stages of dry AMD:
Early stage of dry AMD: People with the early stage of dry AMD have either several small drusen or a few medium-sized drusen. At this stage, there are usually no symptoms or vision loss. It is not certain if having an early stage of AMD puts one at increased risk of developing an intermediate stage of dry AMD.
Early AMD (Credit: National Eye Institute, National Institutes of Health)
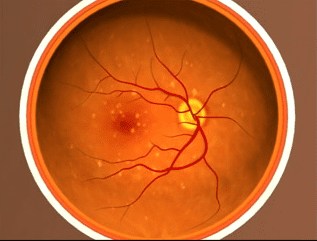
Intermediate stage of dry AMD: People with the intermediate stage of dry AMD have either many medium-sized drusen or one or more large drusen. At this stage, many individuals may still be without symptoms, but some people may see a blurred spot in the center of their vision. Those with the intermediate stage of dry AMD also may require more light or contrast (sharpness between light and dark) for reading and other tasks. They are also at increased risk of developing the advanced stage of dry AMD or developing wet AMD.
Intermediate AMD (Credit: National Eye Institute, National Institutes of Health)
Advanced stage of dry AMD: The advanced stage of dry AMD is also known as geographic atrophy (GA) affecting the fovea or center of one’s vision. At this stage, there are large areas of damaged tissue causing central blind spots. A person may have difficulty reading or recognizing faces.

Dry AMD – Geographic Atrophy (Credit: National Eye Institute, National Institutes of Health)
What is AMD?
Age-related Macular Degeneration, commonly referred to as AMD, affects an estimated 1.8 million Americans aged 40 years and older and an additional 7.3 million with large drusen are at substantial risk of developing AMD. The number of people with AMD is estimated to reach 2.95 million in 2020. AMD if left untreated is the leading cause of permanent impairment of reading and fine or close-up vision among people aged 65 years and older.
AMD affects part of the back of the eye called the macula, which is the central part of the retina (the “film” lining the inside the eye). When AMD damages the macula, the center part of a person’s vision may become blurred or wavy, and a blind spot may develop. AMD can cause vision loss quickly or slowly, and can make it very hard to do things that require sharp central vision, such as reading, crafts, cooking, driving, or recognizing faces; it can also make it difficult to see in dim light. The good news is that AMD almost never causes total blindness, since it usually does not hurt side (peripheral) vision.
What is wet AMD?
Wet AMD, also known as neovascular AMD, generally causes more rapid and more serious vision loss if left untreated. In this form of the disease, people with the intermediate stage of dry AMD or with the advanced stage of dry AMD develop tiny new blood vessels and scar tissue which grow under and into the retina. These blood vessels are fragile and often break and leak, which, along with scarring of the retina, can cause a loss of vision. Wet AMD may be treated with various treatments.
What increases risk for dry AMD?
While the cause of AMD is unknown, some identified which have been identified as increasing risk for AMD include:
- Family history of AMD
- Aging – those over 60 years old
- Race – Caucasians have a higher rate of AMD
- Light colored eyes
- Smoking
- Heart disease
- High blood pressure (hypertension)
- High cholesterol
- Obesity
- High sun exposure
- Poor diet with a low intake of fruits and vegetables (a low intake of anti-oxidants)
What are the symptoms of dry AMD?
There may be no symptoms until the disease progresses or affects both eyes. Vision changes due to dry AMD can include:
- Difficulty seeing in the center of your vision, which is needed for reading, crafts, cooking, recognizing faces, and driving
- Trouble seeing in dim light
- Straight lines start to appear wavy, blurry or missing
- Fading and/or changes in the appearance of colors
If you experience any of these symptoms, see an eye doctor as soon as possible.
How is dry AMD Diagnosed?
The key to slowing or preventing vision loss from dry AMD is regular eye exams. People age 50 or older should get a complete eye exam and follow-up with eye exams every one or two years or as indicated by the eye doctor. It is important to attend all scheduled eye exams even if there are no noticeable vision problems.
During an eye exam, the eye doctor will conduct the following tests:
Visual acuity: This will determine how well a person can see through his or her central vision and if there is a decrease in visual acuity.
Dilated eye examination: The eye doctor will dilate (widen) the pupil of the eye with eye drops to allow a closer look at the back of the eye. The doctor will look for buildup of drusen or a breakdown of pigment and light-sensitive cells in the macula.
Amsler grid: This will test for problems in the macula. An Amsler Grid is made of straight horizontal and vertical lines. AMD may make the straight lines in the grid to appear faded, broken or wavy.
If the eye doctor suspects AMD, then the following tests may be conducted:
Fundus photograph: A fundus photograph provides a picture of the retina and may document the amount of drusen or geographic atrophy to compare at future visits. Sometimes the photograph will be taken with special imaging called autofluorescence, which may help with the identification of geographic atrophy.
Optical coherence tomography (OCT): The OCT examination provides a cross sectional image of the eye, which can show if the macula is thickened, loss of tissue, and/or if there is fluid under the retina that may be affecting vision.
Fluorescein angiography: During this test, a dye is injected into the arm that “lights up” the blood vessels in the eye while multiple photos are taken of the back of the eye. These images might show if there are new blood vessels in the macula and/or if there is leaking of dye (to show there is fluid into or beneath the retina) to determine if an individual has wet AMD.
How is dry AMD Treated?
Supplements: Currently, the only treatment for dry AMD is dietary vitamin and other supplements. A few National Eye Institute (NEI) studies have found that a certain combination of vitamins (vitamins C and E, lutein, zeaxanthin, and zinc), known as AREDS-1 and AREDS-2 (Age Related Eye Disease Study 1 and 2) vitamins, can slow the risk of the intermediate stage of dry AMD to advance stages. NEI researchers recommended a dietary supplement such as that used in these studies, and that cigarette smokers use the AREDS2 study formula. Consult with your health care provider and eye care professional before beginning the supplements. Keep in mind, these vitamins do not cure AMD.
Home monitoring: Those who are at high risk for neovascular AMD are likely to benefit from home device monitoring. A recent study has suggested that using a home monitoring device and program can significantly preserve visual acuity when AMD progressed from dry to wet when compared to those who were using standard care methods alone to self-monitor the progression of their AMD.
Eye exams: An eye doctor may recommend a comprehensive dilated eye exam at least once a year. The exam will help determine if the condition is worsening.
Healthy habits: Healthy habits can lead to healthy eyes – quit smoking, eat healthy and stay active. Talk to a doctor before starting an exercise program.
Low Vision
If you or someone you know has lost some sight to AMD, low vision aids can help you stay independent. Special training, called vision rehabilitation, can provide skills for living with low vision. A low vision specialist will help determine the right combination of aids for your needs. Ask your eye doctor about the possibility of seeing a low vision specialist.
Low vision aids include:
- Magnifying glasses, screens and stands
- Telescopic lenses
- High-intensity reading lamps
- Large-print newspapers, magazines and books
- Close-circuit TVs that magnify a printed page on screen
- Computers and tablets
GuideMe for Age-related Macular Degeneration
Developed by Prevent Blindness, the GuideMe program is a free resource that will ask a few questions about you and your AMD diagnosis. We’ll use your answers to create a customized guide with helpful information, tips, resources and steps you can take to be proactive about protecting your vision and maintaining your quality of life and independence.
Living Well with Low Vision is an online resource to educate those with loss of vision on how maintain their independence and quality of life.